Electrochemotherapy for Dogs & Cats

Written by Courtney Zwahlen, DVM, DACVIM (Oncology)
Electrochemotherapy (ECT) is a local treatment for cancer using a combination of chemotherapy and electric pulse therapy which increases the antitumor effect of the chemotherapy drugs.
The procedure uses short high voltage pulses generated via an electric pulse generator machine. Once the pulses have been delivered, the cell’s plasma membrane has increased permeability to the chemotherapy agent which is administered either intratumorally or intravenously.
The two chemotherapeutics that have shown the most promise and are used most commonly are bleomycin and cisplatin.
- Bleomycin, an antitumor antibiotic, is a hydrophilic drug that has very limited transport through the cell membrane but is extremely cytotoxic once bound to DNA. Bleomycin efficacy appears to be potentiated 1,000 fold with electroporation of cells.
- Cisplatin, a platinum containing chemotherapeutic, also has difficulty getting through the cell membrane but is quite cytotoxic once bound to DNA. Electroporation of cells showed increased cisplatin cytotoxicity up to 80 fold.
Mechanisms of Action
Various mechanisms of action of ECT have been described. Electropermeabilization of the tumor cells leading to increased intracellular drug accumulation, vascular effects, and an increased immune response appear to be the most important.
The principal mechanism of action is increased cellular uptake of bleomycin or cisplatin by exposure of the tumor cells to an electric field (Fig. 1).
The vascular effects include two distinct changes, vascular disruption and vasoconstriction. The vascular disruption involves endothelial cell death and consequently a decrease in local blood flow. The vasoconstriction effect, also known as vascular lock, induces prolonged entrapment of the chemotherapy drug within the tumors.
The last mechanism of action involves antigen shedding by the tumor cells that are destroyed by ECT which can induce some systemic immunity.
Based on the various mechanisms of action of ECT, antitumor activity should be observed in many different types of tumors treated, regardless of their histological type.
An electric pulse applied at the time of maximal drug concentration in the tumor optimizes the antitumor effect. The best timing of the electric pulses for intratumoral administration is immediately after drug injection, whereas for intravenous administration it is 4-8 minutes after drug injection. The drugs remain at a sufficient concentration in the tumor for at least 20 minutes. At longer intervals between electric pulses and chemotherapy administration, the antitumor effectiveness of ECT is decreased. Intratumoral delivery of chemotherapy generates higher drug concentrations locally in the tumor, and lower concentrations in the non-target tissues when compared to intravenous administration. The drug doses are so low whether administered intratumorally or intravenously that they have minimal to no systemic side effects.
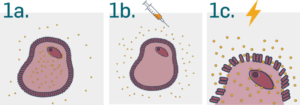
Fig. 1
a. Anticancer drug surrounding the cell
b. Electroporation exposes a cell to a high-intensity electric field that temporarily destabilizes the membrane. During this time the membrane is permeable to the anticancer drug surrounding the cell.
c. When the field is turned off, the pores in the membrane reseal, enclosing drugs inside.
Source: Leroy Biotech
Procedure
The treatment procedure consists of anesthetizing the patient, injecting the chemotherapy either intratumorally and/or intravenously, waiting the appropriate amount of time and then applying the electric pulse (Fig. 2).
In order to get good contact between the electrodes and skin, KY or ultrasound gel is used. Only minor immediate side effects have been noted in people and animals treated with ECT. The most common side effect reported is involuntary contractions/spasms of the underlying muscle in the treated area, but the spasms are only present during the application of the electric pulses. Any associated pain dissipates immediately after the electric pulses are discontinued. Another immediate side effect that has been observed is minor irritation locally.
More delayed side effects can occur and include erythema, edema, and possible necrosis of the tumor. In most cases, patients typically only need one to three treatments, and each treatment under general anesthesia typically takes about 20 minutes. In some cases, tumors may need more than one treatment, especially if the tumors are large.

Fig. 2
a. General anesthesia to ensure security of patient and practitioner.
b. Drug injection: Intratumoral or intravenous injection of cisplatin or bleomycin.
c. Applying electric pulses: 8 pulses of 100 μs every 2 ms (ESOPE standard protocol 2006).
Source: Leroy Biotech
Indications
Electrochemotherapy appears to be a promising and relatively inexpensive local treatment option for dogs and cats with a variety of tumors. It has been utilized for a variety of tumors including squamous cell carcinoma, soft tissue sarcomas, mast cell tumors, localized lymphomas, melanomas, transmissible venereal tumors, perianal adenomas, anal gland adenocarcinomas, sarcoids, and fibropapillomas (Fig. 3-5).
This technique can be used for incompletely excised tumors and/or tumors that cannot be excised without significant complication/deformity to the patient. It can be considered as an alternative to radiation therapy for those patients that are unable to undergo radiation therapy for various reasons.
The treatment can be performed on an outpatient basis, it is safe, and shows good long-lasting objective responses in approximately 80% of patients.
Patients often require 1-3 treatments given once every 2-4 weeks, depending on response.
Local side effects, such as tumor necrosis, are to be expected pending the amount of active tumor that is being treated.
Supportive care, such as bandage changes, anti-inflammatories and antibiotics, are utilized until the treated wound has healed.

Fig. 3
Incompletely excised soft tissue sarcoma over metacarpal region.
Images progress from escar formation, tumor necrosis, debridement and healed wound.
One year later, patient is comfortable with no scar or tumor recurrence.

Fig. 4 Epitheliotrophic Lymphoma affecting lower lip and gingiva.
a. Pre-treatment.
b. Immediately following treatment.
c. 9 days post treatment showing initial tumor necrosis.
d. 12 days post treatment with progressive tumor necrosis.
e. 21 days post treatment, healing mucosa.

Fig. 5 Feline nasal planum squamous cell carcinoma.
A. Before treatment.
B. 2 weeks post.
C. 4 weeks post.
D. 8 weeks post. Complete response >1 year.
Source: Leroy Biotech