A Lameness Puzzle

Presentation and Physical Exam
Daniel, a 3-year-old, male, castrated, Golden Retriever presented to Dr. Kurt Schulz at Peak’s Surgery service for evaluation of a 2 month history of worsening lameness of the right hind leg. Radiographs of the right knee joint had only shown some soft tissue swelling and no other abnormalities. Daniel had no other clinical problems. The lameness improved on Rimadyl.
Physical exam revealed a non-weight bearing lameness of the right hind leg with swelling of the right knee joint. The only other abnormality on physical exam was a II/VI right systolic heart murmur.
Diagnostic work up
Dr. Schulz performed joint taps which showed neutrophilic inflammation of the right knee joint and normal joint fluid cytology in the other joints (total nucleated cell count of 19,490 with 55% neutrophils, 30% large mononuclear cells and 15% small to intermediate size lymphocytes). Culture of the joint fluid was negative.
A vector borne disease profile was submitted to NCSU and was negative for all tested diseases, including tick-borne diseases.
Daniel was transferred to Dr. Marielle Goossens in the Peak Internal Medicine service for further work up of the neutrophilic mono arthritis. A search was started for an underlying disease that could have triggered the neutrophilic inflammation in the right knee joint.
Patient Workup:
- A full profile and urinalysis at Idexx only showed a mildly increased ALT of 145 and the remainder of all values were normal.
- An ultrasound of the abdomen was normal.
- Thoracic radiographs were normal.
- Cardiac work up by Dr. Don Brown showed mild ventricular hypertrophy and some aortic valve insufficiency but no evidence of endocarditis. Systemic blood pressure was normal.
- A Blastomycosis urine antigen test was sent to Mira Vista laboratories and showed a weak positive test, below the limit of quantification.
- After speaking with Mira Vista Diagnostics about these results, Blastomycosis and Histoplasmosis serum antibody EIA testing was performed.
- While waiting for these results, repeat radiographs were obtained of the right knee joint. They showed right stifle effusion and evidence of active osseus lesions at the distal lateral metaphysis and increased medullary opacity, which had not been observed on radiographs 2 months prior (fig. 1).
- A CT and bone biopsy of the right knee joint were performed. Histopathology showed neutrophilic to granulomatous osteomyelitis with new bone formation and osteolysis.
- Special stains were performed for fungal organisms and showed low numbers of broad-based budding fungal organisms, consistent with Blastomyces Dermatitidis (fig. 2).
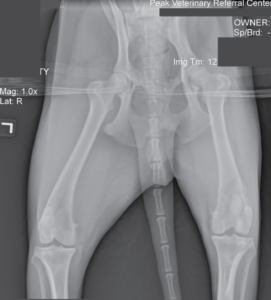
- Fig. 1: Radiograph of the knee joints showing the subtle bone changes in the right knee joint.
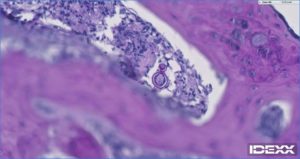
Fig. 2: Histopathology of the bone biopsy showing the broad based fungal organisms consistent with Blastomycosis Dermatitidis.
At the same time as the biopsy results came back, the antibody titers also came back from Mira Vista Diagnostics. The Blastomycosis antibody was negative, but the Histoplasma IgG antibody EIA was high positive.
Treatment and Follow up
Daniel was started on itraconazole after the bone biopsy was taken prior to receiving the results back , as the suspicion for blastomycosis was high. He was treated with generic itraconazole at 5 mg/kg PO once a day. His lameness started to improve within about 2 weeks after starting this treatment and the pain relief medications that he had been on, were gradually discontinued.
Daniel was treated with itraconazole for a total of 8 months. We treated him for 1 month beyond the point of when no further improvement of the boney lesions on the radiographs, could be determined. His urine blastomycosis antigen level had returned to negative prior to this time.
Daniel is now about 2.5 months out after finishing the itraconazole. His first recheck urine antigen level was negative. So far, he is doing well. His urine blastomycosis level antigen test will be performed again at 3, 6, 9 and 12 months after he finished the itraconazole, as relapse of the blastomycosis is common during the first year after finishing treatment. Repeat knee radiographs will also be taken intermittently over this coming year, to make sure that the boney changes remain quiescent.
Case Discussion
Blastomycosis is a diagnosis that is being made more frequently in Vermont and upstate New York over the past several years. What is interesting about Daniel’s case is that he presented with lameness in just one leg and he was not systemically ill. Initially, the only change in him was a swollen, painful knee joint with neutrophilic inflammation in that one joint, with no radiographic changes for the first 2 months of his lameness. We have seen several other cases that presented with neutrophilic inflammation in one joint with or without radiographic changes, that ended up being diagnosed with blastomycosis.
Cases like Daniel’s make us realize, that we need to have the differential of blastomycosis on our rule-out lists for many cases that present to us.
As most of you know, blastomycosis can present itself in our patients in many ways, including:
- Panophthalmitis
- Uveitis
- Mass effects
- Lymphadenopathy
- Draining tracts
- Bone lysis
- Classical presentation of blastomycosis in the lungs (snow storm effect).
The diagnosis is often straightforward by performing the urine blastomycosis antigen test. Sensitivity of this test is over 90%, but false negatives do occur, and we have seen these negatives several times at Peak.
If the urine antigen test is negative, consider cytology and/or histopathology as these techniques are considered the gold standard method for diagnosis. Antibody detection can also be used in antigen negative cases, as we performed in Daniel.
The sensitivity of the AGID method has ranged from 17% to 83% and experience in clinical practice has been unfavorable. The sensitivity of the EIA method is superior to AGID, supporting its use as an aid in the diagnosis of blastomycosis in antigen negative cases.
A Final Note on Blastomycosis
We have seen many cases being treated successfully after the blastomycosis diagnosis. Blastomycosis in the lungs or in the central nervous system, has a higher chance of an unsuccessful treatment. There is evidence that longer treatment may reduce relapse. Relapse rates of 18-25% are listed in the first year after finishing treatment. Recommendations have been made that at least a four to six months course of itraconazole should be given to reduce the likelihood of relapse.
At Peak, we recommended continuing therapy one month beyond resolution of all clinical findings, including eye exam, chest radiographs or bony changes, and one month after the urinary antigen was negative. We then check urine antigen levels at 1, 3, 6, 9, and 12 months after finishing treatment, to make sure we catch a relapse of the blastomycosis prior to the development of symptoms.