Feline Squamous Cell Carcinoma
Katie Cummings, Veterinary Technician Student
A 13-year-old female spayed black domestic long hair presented to The Oncology Service for evaluation after an acute history of blood tinged hyper-salivation and decreased grooming. Her primary veterinarian had noted a granulomatous mass attached to the lingual frenulum and recommended euthanasia.
Examination:
Upon oncologists’ examination, the lingual frenulum mass was noted to be ~1cm in width, causing swelling of the tongue. A grade 2 heart murmur was noted on auscultation. The remainder of her physical exam was within normal limits. The owners elected to move forward with three view thoracic radiographs and sedation to obtain aspirates of the mass for cytology.
The thoracic radiographs showed incidental mild multifocal thoracic spondylosis, but no evidence of pulmonary metastatic disease to the lungs.
Butorphanol 0.4mg/kg and Propofol 2.5mg/kg were given intravenously to induce sedation. The mass was measured, photos were taken, and aspirates were obtained for cytology.

Findings:
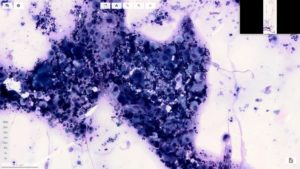
Cytology was diagnostic for oral squamous cell carcinoma, with mild neutrophilic inflammation.
Dr. Obeiter, DVM of Scopio Laboratories, reports:
“The slides are of high cellularity and consist predominantly of round to polygonal squamous epithelial cells seen individually and in cohesive clusters on a background of moderate amounts of blood and associated leukocytes. These cells contain round to ovoid paracentrally located nuclei that measure approximately 2-5x the diameter of a RBC. Nuclei contain lacy chromatin and sometimes contain a variably sized round to ovoid nucleolus. Occasional binucleate and multinucleate cells are seen, some of which display intracellular anisokaryosis. These cells contain moderate to abundant amounts of pale to light blue cytoplasm and sometimes contain small discrete perinuclear cytoplasmic vacuoles. Some cells contain few non-degenerate neutrophils within their cytoplasm (emperipolesis). These cells often display nuclear to cytoplasmic asynchrony and have variable nuclear to cytoplasmic ratios. Occasional mitotic figures, some of which appear bizarre, are present. There is a marked degree of anisocytosis and marked anisokaryosis seen within this population. In some areas, neutrophils appear mildly increased relative to the amount of blood present. Occasional foamy macrophages are also present. Occasional rod-shaped bacteria are seen extracellularly and adhered to squamous cells. No bacteria are observed intracellularly within neutrophils.”
Recommendations:
Multiple different therapeutic options are available for this tumor type, but only surgery can provide long term control. Unfortunately, due to the location of the mass in this case, surgery would not provide complete excision of the mass.
However, an accelerated radiation protocol for oral squamous cell carcinoma could provide median overall survival of 86-110 days. Palliative radiation can also be considered, but data suggests there is no improvement in comfort in cats with inoperable oral squamous cell carcinoma. Palladia, in conjunction with Piroxicam/other NSAIDs, can have a considerable improvement in survival time. Despite this, long-term survival time remains poor.
After diagnosis and discussion with owners, they elected palliative care with oral Buprenorphine at 0.1mg/kg and Magic mouthwash (1 part oral diphenhydramine, 1 part aluminum hydroxide, 1 part lidocaine) oral suspension. 30mLs of subcutaneous fluids were administered at the request of the owner.
References:
Fidel, Jeanne N. et all, “A Nine-Day Accelerated Radiation Protocol for Feline Squamous Cell Carcinoma” The Official Journal of the American College of Veterinary Radiology, Vol. 48, Iss. 5
Bregazzi, Victoria S. et. all “Response of Oral Squamous Cell Carcinoma to Palliative Radiation Therapy” Veterinary Radiology and Ultrasound, Vol. 48, Iss. 1
Valerie Wiles et. All “Retrospective Evaluation of Toceranib phosphate (Palladia) in Cats with Oral Squamous Cell Carcinoma” Journal of Feline Medicine and Surgery, Vol. 19, Iss. 2